Medication adherence improves overall patient health and reduces hospitalizations
Non-adherence takes the lives of 125,000 Americans each year and costs the healthcare system nearly $300 billion a year in additional medical visits and hospitalizations. (Source: American Heart Association)
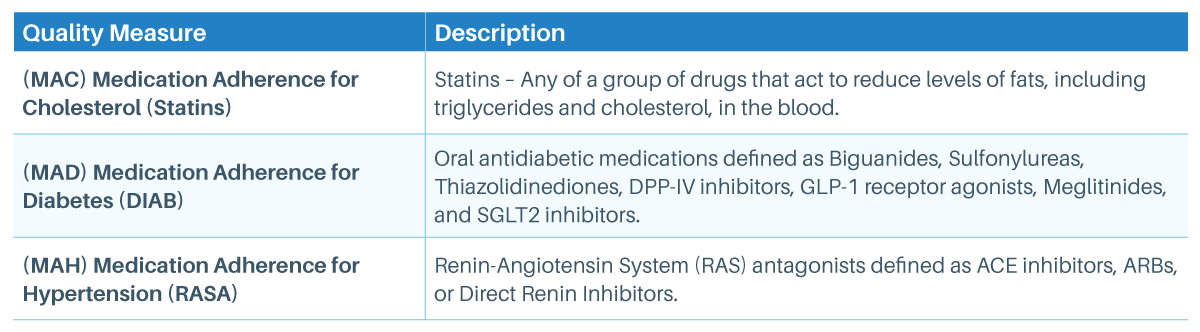
Focus on these Medication Adherence Measures for MEDICARE PART D
- (MAC) Medication Adherence for Cholesterol Medication (Statins)
- (MAD) Medication Adherence for Diabetic Medication
- (MAH) Medication Adherence for Hypertension (RAS Antagonists) Medications
Measure Compliance
Percent of members ages 18 and older who adhere to their medication at least 80% of the time in the measurement period.
Measure Tips
- Members qualify for the measure with the 2nd fill, but the measurement period starts with the date of the 1st fill.
- To be included in the measure, the 1st fill of medication must occur at least 91 days before the end of the enrollment period.
- The proportion of days is the percent of days in the measurement period covered by prescription claims for the same medication or another in its therapeutic category.
Measure Exclusions
- Members in Hospice
- End-Stage Renal Disease (ESRD), or on dialysis
- For Diabetes (MAD): One or more prescription claims for Insulin
- For Hypertension (MAH): One or more prescription claims for Sacubitril/ Valsartan (Entresto®)
Best Practices
Order 90-day prescriptions
Enrolling in 90-day or home delivery programs can ensure compliance.
Review ALL medications
During each visit, including over-the-counter. When feasible, reduce medications/dosages.
Ensure understanding
Purpose of medication, potential side effects, how to manage
Common Concerns and Discussion Points
Cost too high
Recommend generic or combo drug(s)
Transportation issues
Check whether the member’s pharmacy offers delivery; for mail service:
- Emblem: (877) 866–5828 (Express Scripts)
- Anthem: (833) 207–3117 (Carelon)
Unable to manage or remember
- Help to set up a phone alarm and other tools, e.g. pill box organizer.
- Encourage members to enroll in a refill reminder program with their pharmacy or at-home delivery.
- Limit prescription frequency to a maximum of twice per day, when possible.
Worried about side effects/not working
- Explore additional options
- Explain importance/purpose of drug
HealthCare Partners (HCP) is here to help!
HCP Pharmacy Staff
Call: (516) 515–8861
Monday through Friday, 8:30am – 5:30pm EST
HCP Case Managers
Call: (888) 258–0203
Monday through Friday, 8:30am – 5:30pm EST
Our Case Managers can:
- Teach patients about their condition.
- Guide them in making a treatment plan.
- Help them get medications and care.
- Coordinate transportation based on member’s assigned benefit.
- Set up referrals and doctor visits.
- Provide a Nurse on call, 24/7 at (516) 238-6124.
Download Medication Adherence








